Facial atopic dermatitis (AD), often referred to as facial eczema, is more than a cosmetic concern. Because the skin on the face is thin, constantly exposed to environmental triggers, and closely associated with psychological wellbeing, flare-ups here can cause significant discomfort and emotional distress. Managing facial AD requires a balance of effective medical therapy, careful skincare practices, and long-term preventive strategies. This article provides a comprehensive guide on how to treat facial atopic dermatitis, covering everything from everyday routines and medical treatments to advanced systemic options and lifestyle adjustments.
Related Article: How to Use Blackhead Remover Safely & Effectively for Clear Skin
Recognize Symptoms of Facial Atopic Dermatitis Early
Facial atopic dermatitis typically presents with redness, itching, flaking, and sometimes oozing or crusting, particularly around the eyes, mouth, and cheeks. Because the face is highly vascular and sensitive, even mild inflammation becomes visible quickly, which makes early recognition important. Prompt attention can prevent progression into more severe stages.
The key diagnostic elements include persistent itching, symmetrical patches, chronic or relapsing flares, and a personal or family history of allergies or asthma. Unlike acne or seborrheic dermatitis, facial AD usually involves dryness and worsens with irritants like soaps or perfumes.
Left untreated, the condition may lead to secondary infections, pigment changes, or scarring, which are particularly concerning on facial skin. Early treatment not only improves skin health but also protects long-term psychological wellbeing, as visible skin diseases strongly affect self-esteem.
Cleanse Facial Skin Gently and Correctly
The foundation of managing facial AD is gentle cleansing without stripping the skin barrier. Harsh soaps, foaming cleansers, or exfoliants often aggravate symptoms by removing natural oils. Instead, dermatologists recommend pH-balanced, fragrance-free, non-foaming cleansers that leave a thin protective film on the skin.
The process matters as much as the product: use lukewarm water, apply cleanser with fingertips instead of scrubs, and gently pat dry with a soft towel. Over-washing should be avoided, as frequent cleansing increases transepidermal water loss.
Consistency in cleansing routines reduces flare frequency. In environments with hard water or pollution, double-rinsing with filtered water can further minimize irritation. For infants and children, cleansing should be minimal, often limited to once daily, with extra care to avoid rubbing.
Moisturize with Barrier-Repair Formulations
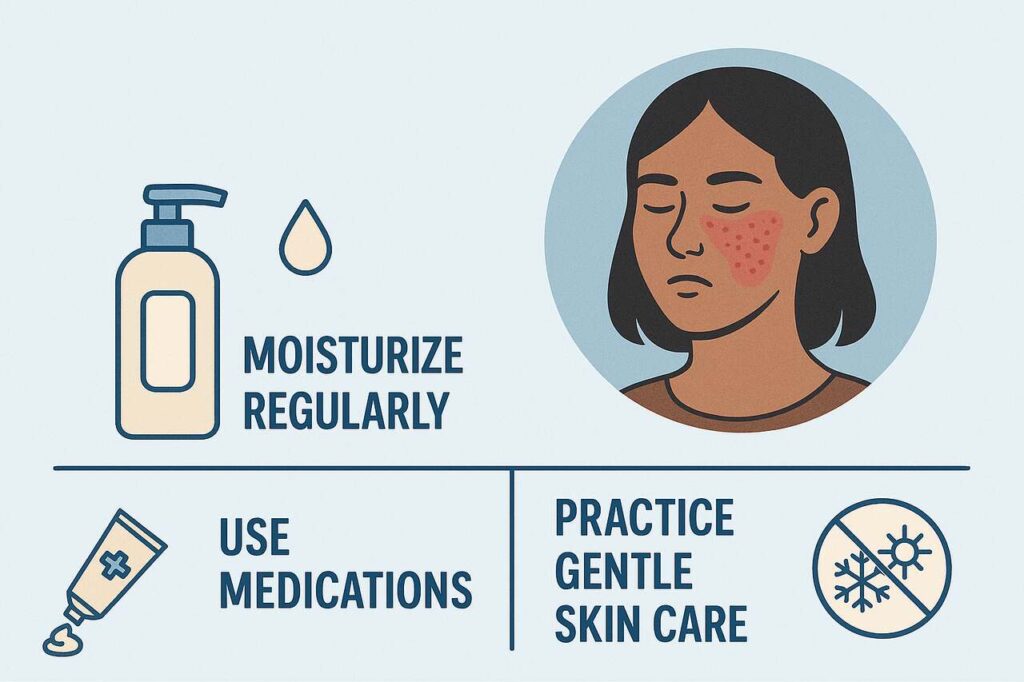
Moisturization is the cornerstone of facial AD care. Since the disease involves a defective skin barrier, regular emollient use helps restore hydration, reduce itching, and extend remission between flares.
The most effective moisturizers contain occlusive agents (petrolatum, dimethicone), humectants (glycerin, hyaluronic acid), and lipid-replenishing ceramides. Facial formulations should be lightweight yet protective, avoiding alcohol, fragrances, and lanolin which may trigger reactions.
Application timing is crucial: moisturizers should be applied within three minutes of cleansing to lock in water. Layering is also helpful for example, applying a gel-based hydrator followed by a thicker cream to seal the barrier. With consistent use, barrier repair reduces the need for stronger medications.
Use Topical Corticosteroids Safely on the Face
Topical corticosteroids remain first-line for flare control, but special caution is required on facial skin due to its thinness and sensitivity. Only low- to mid-potency steroids (e.g., hydrocortisone, desonide) are recommended, and typically for short bursts of 1–2 weeks.
Prescribing guidelines emphasize fingertip-unit dosing to avoid overuse. Potent steroids may sometimes be used under close supervision for severe flares, but chronic use risks skin thinning, pigment changes, telangiectasia, and steroid-induced rosacea.
Because many patients fear steroid side effects, some delay treatment, which allows inflammation to worsen. Educating patients about safe use protocols short courses, low potency, and medical supervision helps balance effectiveness with safety.
Apply Topical Calcineurin Inhibitors as Steroid-Sparing Options
For long-term or sensitive-site use, topical calcineurin inhibitors (TCIs) such as tacrolimus (Protopic) and pimecrolimus (Elidel) are often preferred. They suppress immune activity without the thinning effects of steroids, making them ideal for eyelids, lips, and cheeks.
TCIs are applied twice daily during flares, then reduced to proactive use twice weekly to prevent relapses. Patients may initially experience a burning sensation, which usually subsides within a week.
In clinical trials, tacrolimus has shown comparable efficacy to mid-potency steroids for facial AD, with much safer long-term profiles. TCIs also improve patient confidence by offering a steroid-free maintenance strategy, especially important for chronic facial involvement.
Consider Non-Steroidal and Novel Topical Therapies
Beyond TCIs, new non-steroidal topicals are expanding treatment options. Agents like crisaborole (Eucrisa), a PDE-4 inhibitor, reduce inflammation with minimal local side effects. Emerging creams such as tapinarof (Vtama) show promise by modulating the aryl hydrocarbon receptor pathway.
These treatments provide alternatives for patients resistant to or fearful of steroids. They can be safely combined with emollients and used in children or adults.
While accessibility and cost remain challenges, especially outside North America and Europe, the growing pipeline of non-steroidal topicals reflects a shift toward barrier-repair and inflammation-modulating therapies that are safer for long-term facial use.
Escalate to Systemic Therapy When Needed
For moderate-to-severe facial AD that fails topical care, systemic treatment becomes necessary. Dupilumab, the first biologic approved for AD, targets IL-4/IL-13 pathways and has shown dramatic improvements in facial lesions. Other biologics, such as tralokinumab and lebrikizumab, are expanding options.
Additionally, oral JAK inhibitors (abrocitinib, upadacitinib, baricitinib) provide rapid relief for severe cases, though long-term safety monitoring is essential. These are usually reserved for patients whose disease significantly impairs quality of life or function.
Because systemic agents carry higher costs and require monitoring, dermatologists assess candidacy carefully. However, their arrival marks a breakthrough: for the first time, patients with refractory facial AD can achieve near-clear skin.
Identify and Avoid Common Triggers
Treatment is incomplete without trigger management. On the face, common irritants include fragranced cosmetics, harsh cleansers, sunscreens with chemical filters, and environmental exposures like dust or smoke. Stress, lack of sleep, and sweating also commonly worsen symptoms.
Identifying triggers often requires patient diaries and sometimes patch testing. For children, food allergens may occasionally contribute, though routine elimination diets are not advised without professional guidance.
Proactive avoidance of triggers helps reduce medication reliance. For example, switching to mineral sunscreens, hypoallergenic moisturizers, and fragrance-free cosmetics can dramatically reduce flare frequency in sensitive individuals.
Protect Facial Skin from Sun and Environmental Stressors
Photoprotection is especially important because facial AD skin is both sensitive and exposed. Sunscreens should be broad-spectrum, SPF 30 or higher, and preferably mineral-based (zinc oxide or titanium dioxide) to minimize irritation.
Protective clothing, hats, and avoiding midday sun also reduce risks. Seasonal factors matter: cold dry winters and hot humid summers both worsen facial AD, requiring tailored adjustments like humidifiers or lighter formulations.
Environmental pollutants may exacerbate inflammation by disrupting the microbiome. Gentle cleansing and barrier-strengthening products provide defense. Over time, consistent protection supports not just disease control but also cosmetic outcomes such as preventing post-inflammatory pigmentation.
Compare Treatment Options for Facial AD
| Treatment Category | Examples | Benefits | Risks / Limitations | Best Use Case |
| Topical Steroids | Hydrocortisone, desonide | Rapid flare control | Skin thinning, pigment changes, rebound flares | Short-term flare management |
| Calcineurin Inhibitors | Tacrolimus, pimecrolimus | Safe long-term use, ideal for sensitive sites | Initial burning, higher cost | Maintenance, eyelids, chronic disease |
| Non-Steroidal Topicals | Crisaborole, Tapinarof | Anti-inflammatory, steroid-free | Cost, limited access | Patients intolerant to steroids |
| Biologics | Dupilumab, Tralokinumab | High efficacy, systemic relief | Expensive, injection route | Moderate-to-severe refractory cases |
| JAK Inhibitors | Upadacitinib, Abrocitinib | Rapid itch reduction | Safety monitoring needed | Severe disease requiring systemic control |
Support Mental Health and Quality of Life
Because the face is central to identity, visible dermatitis can cause self-consciousness, anxiety, and depression. Studies show that children and adults with facial AD report greater social withdrawal and bullying than those with eczema on covered sites.
Holistic management should include psychological support whether through counseling, support groups, or stress-reduction strategies like mindfulness. Adequate sleep, exercise, and balanced diet also reduce flare triggers while supporting overall resilience.
Acknowledging the emotional burden validates patient experiences and strengthens adherence to treatment plans. A dermatologist who addresses both medical and psychosocial aspects provides the most comprehensive care.
Read Also: You Might Be Missing the Biggest Mental Benefit of Exercise: Here’s Why It Matters
Conclusion
Treating facial atopic dermatitis requires a multi-layered approach: gentle skincare routines, evidence-based topical therapies, timely escalation to systemic agents when necessary, and consistent trigger avoidance. Because the face is both sensitive and socially important, safety and cosmetic outcomes carry special weight. Advances in non-steroidal topicals and biologics now offer long-term solutions beyond steroids, while supportive care helps patients maintain confidence and quality of life.
By combining medical expertise with personalized routines and lifestyle adjustments, individuals with facial AD can achieve sustained control, healthier skin, and improved wellbeing. For more informative articles related to Beauty’s you can visit Beauty’s Category of our Blog.
FAQ’s
Mild topical steroids are generally safe for 1–2 weeks during flares. Long-term or potent steroid use risks skin thinning and should be avoided without medical supervision.
Options include calcineurin inhibitors (tacrolimus, pimecrolimus), crisaborole, and newer agents like tapinarof. These provide long-term safety without thinning the skin.
Apply fragrance-free, ceramide-rich moisturizers immediately after cleansing. Avoid products with alcohol, strong preservatives, or fragrances that may irritate.
Yes. Certain ingredients—especially chemical filters, fragrances, and preservatives—are common triggers. Safer options include mineral sunscreens and hypoallergenic cosmetics.
If facial AD remains moderate-to-severe despite proper topical care, or if flares are frequent and impair quality of life, systemic therapy should be discussed with a dermatologist.
Maintaining indoor humidity, reducing stress, avoiding extreme weather exposure, and using gentle skincare products can all help.
Some patients benefit from identifying specific triggers, but broad food elimination is not universally effective. Allergy testing should be guided by a professional.